The effects of smoking during pregnancy is a widely researched topic with one common finding: pregnancy and cigarette smoke don’t mix.
Even if you are not a smoker, inhaling cigarette smoke exposes you and your unborn child to all sorts of scary things that any expectant mom fears during her pregnancy including miscarriage, stillbirth, preterm birth, and sudden infant death syndrome.
But I bet the crippling fear of an expectant mom is seeing her child go through a horrible life because of a mistake that she made.
| Are you an expectant parent? On my website you can find many tips for first-time parents, baby products reviews and summaries of recent scientific studies about pregnancy and parenthood. |
No Buts About It
What’s so disturbing is that despite the well-understood risks of smoking on pregnancy and development of the baby, this is still a significant health concern today.
It’s undeniable that smoking is far much less common than it was a decade ago. However, the latest findings from a study on the prevalence of smoking during pregnancy show that 1 in every 14 expectant women in the USA in 2016 smoked cigarettes.
Precisely, the data, collected by the Centers for Disease CDC’s National Center for Health Statistics show that 7.2% of the pregnant women in that year smoked.

This study also found out that the prevalence of smoking during pregnancy varied from state to state. For instance, West Virginia recorded the highest rate at 25.1%, while only 1.6% of expectant women smoked in California.
The report also shows that the prevalence of smoking varied widely according to age. Women between 20 and 24 years had the highest prevalence at 10.7%, followed by those in 15-19 age bracket at 8.5%, and 25-29 years at 8.2%. Smoking when pregnant was less prevalent among women above 45 years at 2% and those who were below 15 years (2.5%).
The results also varied significantly according to maternal race and Hispanic origin. Non-Hispanic American, Indian, and Alaska Native women recorded the highest smoking rate while pregnant at 16.7%. Non-Hispanic black women and non-Hispanic white women came 2nd and 3rd at 6% and 10% respectively. Lastly, Hispanic and non-Hispanic Asian women were the least likely to smoke at 1.8% and 0.6% respectively.
In terms of education level, the prevalence was lowest among women who had a bachelor’s degree only at 1%, followed by those who had a master’s degree or higher (4%). Women with GED or a high school diploma were the most likely to smoke while pregnant at 12.2%. They were followed by those who had attained lower than a high school diploma (11.7%). Women with college and associate’s degree had a prevalence of 7.9%.
The major limitation that the researchers reported was that all the data obtained for this study was based on self-reports. Because of the negative attitude towards smoking during pregnancy, the researchers state that most women might not admit that they smoked while expectant. And that’s to say that the prevalence may be underreported.
Effects Of Smoking On Mother & Baby: Scientific Research Findings
Studies on maternal smoking have been done on 2 major categories:
- Effects on fertility and pregnancy complications,
- Short-term and long-term effects of smoking on the child’s development.
We will discuss both these categories below.
Effects On Fertility & Pregnancy Complications
One study analyzed current literature with the aim of understanding the risks of maternal smoking and pregnancy outcomes. These were the general findings:
Delayed Conception And Infertility
This meta-analysis found out that smokers had a much lower pregnancy rate compared to non-smokers. Report findings cited in this study showed that smokers had the highest odds of infertility at 95% compared to non-smokers. In addition, sub-fertile women who smoke and who were undergoing vitro fertilization (assisted reproductive technology) were found to have reduced ability to conceive.
Explaining these findings, the researchers state that cigarette smoke appears to have estrogen-blocking effects. Estrogens are sex hormones that help in regulating menstruation.
They also go ahead to explain that nicotine- the main ingredient in tobacco- as well as other toxic products produced during cigarette combustion may interfere with the development of the corpus luteum, tubal transportation system, and implantation.
This explains why experts advise women who want to conceive to give up smoking earlier.
Ectopic Pregnancy
This study also found a strong correlation between smoking and an increased risk of ectopic pregnancy. Ectopic pregnancy is where implantation takes place outside the uterus and mostly in the fallopian tube. This is a high-risk condition that is leading in maternal deaths in the US.
In another study carried out by experts from Edinburgh University and published in the American Journal of Pathology, the researchers found out that cotinine – the end product of nicotine- increased the production of a protein called PROKR1.
The researchers argue that the increased level of this protein in the fallopian tubes prevents the contraction of the muscles in the tubes thereby hindering the movement of the egg to the womb.
This was after they found twice as much PROKR1 proteins in smokers who developed ectopic pregnancy than non-smokers who had had a healthy pregnancy before.
Other external studies show that cigarette smoking increases the odds of ectopic pregnancy by up to 4%. If not dealt with in time, this condition can cause the fallopian tubes to rupture thereby leading to internal bleeding. This may also cause fertility problems in the future or even lead to maternal death.

Placental Abruption
This is a complication where the placenta detaches prematurely from the uterine wall before childbirth thereby depriving the fetus of oxygen and nutrients.
Placental abruption is a serious condition that can lead to severe bleeding thereby endangering the life of the mother and the unborn child. This is because there’s currently no way to reattach the placenta once it separates from the rig.
Smoking during pregnancy has been repeatedly associated with placental complications with smokers facing a twofold increased risk compared to non-smokers.
In-depth studies on how cigarette smoking increases the odds of placental abruptions reveal several possible mechanisms:
- Toxins in cigarette smoke have been found to cause degeneration and inflammations on the surface of the placenta,
- Smoking is also associated with lower levels of plasma ascorbic acid- this may lead to premature separation of the placenta from the uterus,
- It has also been found to cause the membranes to rupture prematurely thereby elevating the risk of placental abruption.
An important finding here is that the risk of placental abruption increases with the number of cigarettes smoked. Generally, expectant women who smoke more tend to have a higher risk compared to those who smoke less. In addition, smokers who quit during pregnancy lower their risk compared to those who continue smoking.
Placenta Previa
Placenta previa is another complication that occurs when the placenta fails to grow towards the upper part of the uterus and instead remains in the lower part. As a result, it covers the opening of the cervix either wholly or partially thereby making it impossible to deliver the baby normally.
This condition can also lead to severe bleeding without pain before or during delivery. It also increases the risk of preterm and maternal deaths as well as perinatal death.
Yes, smoking has been found to increase the risk of placenta previa by between 1.5 and 3. It does this by increasing the level of carbon monoxide at the expense of oxygen. And that’s to say that the blood has far much less oxygen in smokers than in non-smokers. This condition is called chronic hypoxemia and it’s known to cause the placenta to enlarge and cover the cervix.
Effects Of Smoking On The Baby
Stillbirth
There is strong biological evidence that smoking can cause the death of the fetus after 28 weeks of pregnancy. Studies show that this risk increases with an increase in exposure to nicotine. An expansive study conducted in 30 developing countries found out that in Pakistan, over 40% of all expectant moms are exposed to second-hand smoke that causes approximately 17,000 stillbirths per year.
Researchers explain that the risk of stillbirth is largely caused by smoking-related hypoxemia (low concentration of oxygen in blood), increase in vascular resistance, placental abruption, and placenta previa.
A Danish study has some good news, though. It found out that expectant women who stopped smoking during the first months of pregnancy lowered this risk to that of non-smoking mothers.
Neonatal Mortality
This refers to the death of a newborn during its first 28 days of life. While there are lots of other reasons that may lead to neonatal mortality, the risk has been found to be significantly higher among babies born by smoking mothers.
In a Swedish study done between 1983 and 1985 and which involved 281,808 births, the overall rates of neonatal mortality and late fetal death were 3.1 and 3.5 for every 1,000 deaths. A significant finding here was that 30% of the moms reported being daily smokers.
Increased Risk Of Oral Cleft
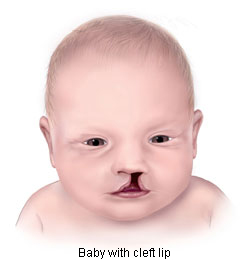
An oral cleft is a birth defect that occurs when a baby’s 2 parts of the upper lip fail to join together completely in the first trimester. This is usually caused by lack of enough tissue in the lip area and may lead to speech problems, frequent ear infections, and difficulties in feeding.
Although diabetes, giving birth at old age, obesity, and certain medications have been associated with oral clefts, smoking during pregnancy is often cited as the first risk factor.
A Norwegian study cited by Science Daily aimed at identifying the link between smoking and oral clefts. It included 573 babies with oral cleft and 763 others who had been randomly selected as controls.
The results of the study showed that smoking cigarettes increased the risk of cleft lip by almost 2-fold when the moms smoked over 10 cigarettes during the first trimester. This risk fell to around 1.6 fold for mothers who were exposed to passive smoke.
Although researchers haven’t understood clearly how smoking causes oral cleft, they explain that the genes that are involved with the detoxification of cigarette smoke in the body don’t appear to be the cause.

Long-term Effects Of Maternal Smoking On Children
Later Obesity
Maternal smoking has consistently been found to have a direct link to low birth weight. And unlike previous claims, recent studies show that this is caused by the hypoxic effects of carbon monoxide as opposed to reduced maternal appetite.
But another effect that seems rather counterintuitive is that babies exposed to cigarette smoke in the uterus have a higher risk of obesity coupled with metabolic disorders. This is according to findings from a recent meta-analysis of studies published in the National Institutes of Health.
In an attempt to explain how cigarette smoke could lead to weight gain, experts state that utero nicotine exposure could alter hypothalamic regulation of energy intake and expenditure. In addition, nicotine is also thought to lead to abnormal cell differentiation, proliferation and synaptic activity in the brain.
Future Cardiovascular Problems
The study above also shows that smoking when pregnant affects the offspring’s cardiovascular health. Prenatal exposure has been associated with lower Fetal Heart Variability in the uterus. After birth, several studies including this one have found that prenatal maternal smoking could alter with blood pressure during childhood.
This study goes ahead to prove that these effects could be persistent even in adolescence. But what’s more strange is that some findings show that smoking could negatively affect the child’s BP even if the mother quits smoking months before conceiving.
Later Respiratory Illnesses & Problems
Utero tobacco exposure has also been linked to an increased risk of asthma, airway hyperresponsiveness, wheezing, bronchitis, and impaired lung function. Research studies show that the risk of asthma and wheezing remains high among kids below 2 years and could persist up to adolescence and an age of up to 18 years.

When And How To Quit Smoking During Pregnancy
It’s evident from all the studies above that when you smoke during your pregnancy, so does the child in your womb. And as we’ve just seen, the effects of maternal smoking can persist up to adolescence.
If you are a smoker and are planning to get pregnant, the best time to quit is at least 3 months before conceiving.
Experts advise that it’s never too late to quit especially when expectant. Women who stop smoking when already pregnant have been found to lower the dangers of maternal smoking by a higher rate compared to those who don’t.
Smoking cessation might seem hard at first, but it’s doable if you are determined. In addition, there are lots of support programs that help expectant moms in this journey. The Centers for Disease Control and Prevention, for instance, has a team of quit coaches on their quitline 1-800-QUIT-NOW (1-800-784-8669) who support and help smokers develop a quit plan.
Smokefree Women also offers a lot of information on this issue and may also offer free or low-cost quit counseling and/or medication.
Importantly, you could also ask for help from your doctor and seek for tips from former smokers (friends and relatives) who made it.
If you are already pregnant, you should definitely consult all of this with your gynecologist, to make sure your lifestyle doesn’t expose your unborn child to any danger. In many cases quitting smoking requires medical supervision.
Bibliography:
Banderali, G., et al. “Short and long term health effects of parental tobacco smoking during pregnancy and lactation: a descriptive review.” Journal of translational medicine 13.1 (2015): 327.
Cnattingius, Sven. “The epidemiology of smoking during pregnancy: smoking prevalence, maternal characteristics, and pregnancy outcomes.” Nicotine & tobacco research 6. Suppl_2 (2004): 125-S140.
Cnattingius, Sven, Bengt Haglund, and Olav Meirik. “Cigarette smoking as risk factor for late fetal and early neonatal death.” BMJ 297.6643 (1988): 258-261.
Drake, Patrick, Anne K. Driscoll, and T. J. Mathews. “Cigarette smoking during pregnancy: United States, 2016.” (2018).
Högberg, Lovisa et al. “Effects of maternal smoking during pregnancy on offspring blood pressure in late adolescence.” Journal of hypertension vol. 30,4 (2012): 693-699. doi:10.1097/HJH.0b013e32835168f4
Meyer, Mary B. “How does maternal smoking affect birth weight and maternal weight gain?: Evidence from the Ontario Perinatal Mortality Study.” American journal of obstetrics and gynecology 131.8 (1978): 888-893.
Oken, Emily et al. “Associations of maternal prenatal smoking with child adiposity and blood pressure.” Obesity research vol. 13,11 (2005): 2021-8. doi:10.1038/oby.2005.248
The purpose of this article is informative. It is a summary of the latest research results and it’s not a substitute for consultation with a doctor. Always consult your health concerns and decisions with your doctor.

